Tudor Hart’s inverse care law classically described that those with the greatest need, paradoxically, often receive the poorest health care. This is a stark reality for the estimated 450,000 Australians with intellectual disabilities, who are at significantly higher risk of chronic disease, neglected mental health challenges and preventable poor health outcomes.1
Despite this, they are far less likely to access preventative health services, with only 10% completing an annual Medicare-funded health assessment, compared to 22% of the general population.2 Life expectancy for people with intellectual disabilities remains up to 27 years shorter than the general population, underscoring the need for urgent systemic and practice-level change.2
Lived experience matters
Hear firsthand from individuals with intellectual disabilities as they share their experiences in accessing healthcare.
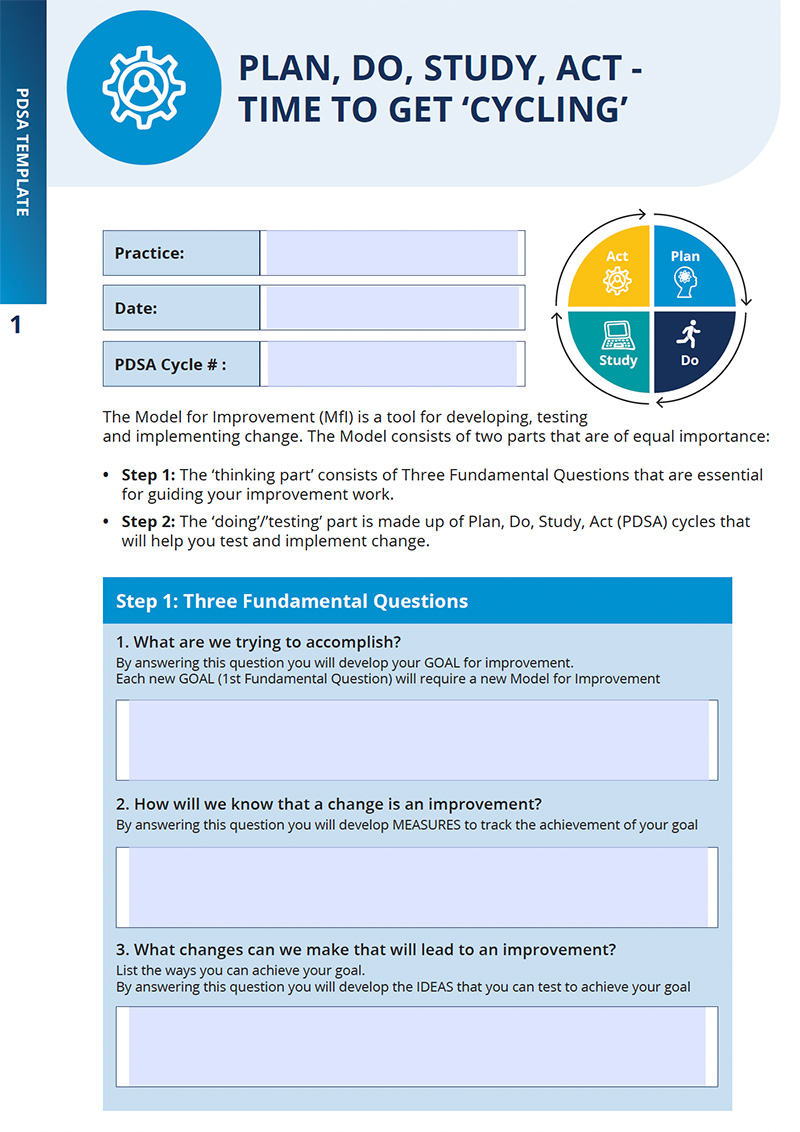
At the heart of this challenge is the opportunity for improvement. By prioritising QI initiatives, your practice can be a leader in delivering patient-centred, inclusive, and comprehensive care to individuals with intellectual disabilities. Through embedding structured QI processes, clinicians and staff will feel better supported to address complex needs and overcome barriers to care.
CCQ is committed to improving healthcare outcomes for people with intellectual disabilities through the Primary Care Enhancement Program (PCEP) as part of the Australia Government’s National Roadmap for Improving the Health of People with Intellectual Disability. Check out what we’ve been up to.