Why bowel screening matters
Bowel cancer is one of the most common cancers in Australia, and we have one of the highest rates globally. When found early, more than 90% of cases can be successfully treated.1
The National Bowel Cancer Screening Program (NBCSP) recommends completing the free iFOBT test every two years, sent to eligible people aged 50–74. As of 2024, the eligibility age has been lowered to 45 — people aged 45–49 can now request their first kit through a simple online order form.
Private kits are not recommended for routine screening, as they are not tracked by the national program.
Where our region is falling behind
Participation in bowel screening is declining nationally — from 43.8% (2019–20) to 40.9% (2020–21).2
In the CCQ region, rates sit just below at 40.8%, with Central Queensland at 34.5%.2
Screening rates are lowest among:3
- People aged 45–55 (especially men)
- Aboriginal and Torres Strait Islander peoples
- Culturally and linguistically diverse communities
- People with disabilities
- Those experiencing social disadvantage
The role of general practice
Primary care providers play a critical role in improving screening rates through the National Bowel Cancer Screening Program through:
- Trusted patient relationships
- Accessibility and preventative care delivery
- Opportunistic screening during routine appointments
Research shows that strong primary care involvement is directly linked to increased cancer screening participation.
Healthcare providers can now bulk order and issue bowel screening kits directly to their eligible patients through the alternative access to kits model. This is in addition to the existing mail out model. See below resources for more information.
How this toolkit supports your practice
This QI Toolkit helps your practice:
- Identify eligible patients
- Set achievable goals and track your progress
- Access tailored tools, data reports, and support
- Engage your team and embed improvements into everyday care
📢 New local consumer campaign (late May/June)
CCQ has developed a bold consumer-facing bowel screening campaign targeting 45–49 year old men; a group with particularly low participation rates.
The Post Your Poo campaign will launch in late May and run throughout June, using humour, cut-through and community engagement to shift perceptions and drive screening uptake.
We encourage practices to align their efforts with this public campaign to help reinforce key messages and encourage follow-through from patients.
Together, we can create a consistent, memorable message and lift bowel screening rates where they matter most.
Digital Campaign Resource Kit for general practice coming soon!
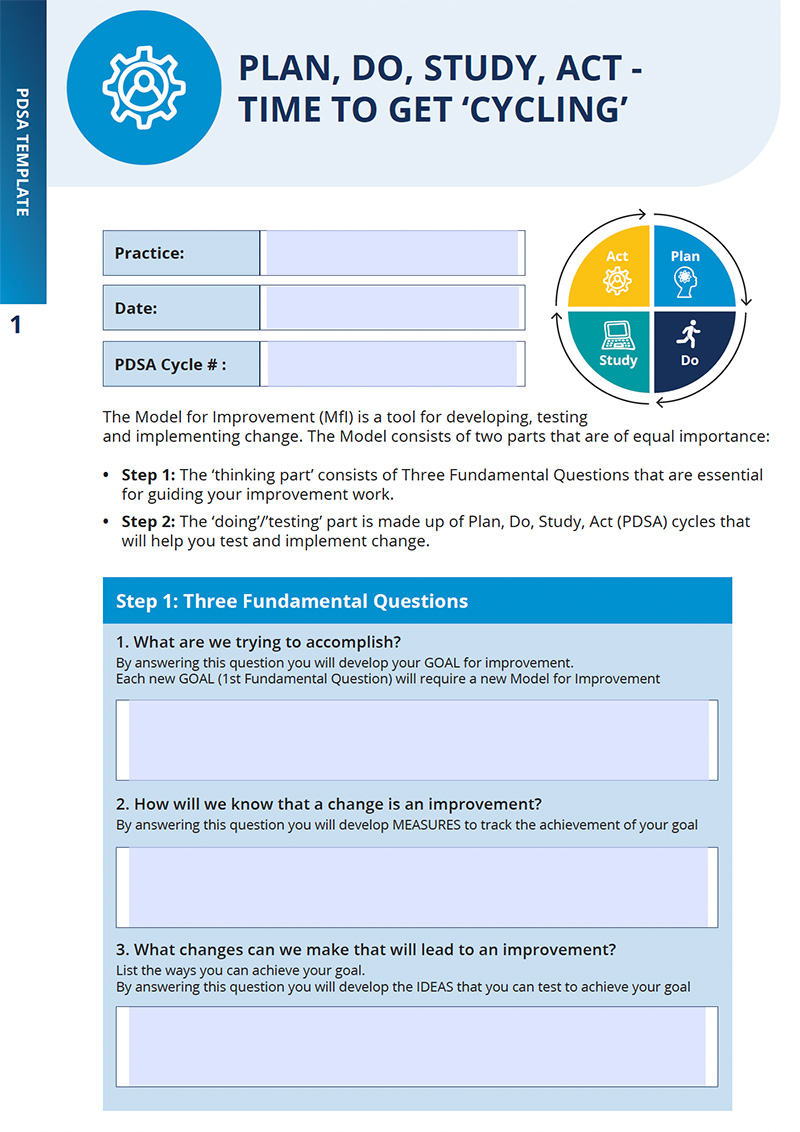
The National Bowel Cancer Screening Program (NBCSP) plays a critical role in reducing mortality by supporting early detection through the free immunochemical faecal occult blood test (iFOBT). With recent updates lowering the eligibility from 50 to 45, the program now enables earlier engagement in screening.
The participation rate in bowel cancer screening has dropped from 43.8% in 2019–2020 to 40.9% in 2020–2021.2 The CCQ region sits just below at 40.8% participation, however, noting the lowest participation rates occurring in Central Queensland at 34.5% on average.1 Screening rates are lowest amongst the following population groups: those aged 45-55, particularly men, Aboriginal and Torres Strait Islander peoples, culturally and linguistically diverse communities, people with disabilities and those experiencing social disadvantage.3
Primary care providers play a critical role in driving bowel screening participation through their trusted relationships, clinical expertise and accessibility to engage patients in preventative care. Research suggests that strong primary health care involvement is associated with greater cancer screening participation rates.3
This QI Toolkit focuses on how to identify and engage eligible patients in bowel cancer screening and increase participation rates in your practice.
📢 New local consumer campaign (May/June)
CCQ has developed a bold consumer-facing bowel screening campaign targeting 45–49 year old men; a group with particularly low participation rates.
The Post Your Poo campaign uses humour, cut-through messaging and community engagement to shift perceptions and drive screening uptake.
We encourage practices to align their efforts with this public campaign to help reinforce key messages and encourage follow-through from patients.