Diabetes remains a critical health challenge in Australia. Between 2000 and 2021, the age-standardised incidence rate for type 2 diabetes declined by 43%1 reflecting significant advancements in prevention through improved screening, increased public awareness, and educational programs fostering behavioural change.2 However, despite these gains, the absolute burden of diabetes continues to grow.
The number of Australians living with diabetes has surged nearly 2.8-fold during the same period, rising from 460,000 to 1.3 million.1 By 2024, type 2 diabetes accounted for around 128,000 years of healthy life lost,1 highlighting the persistent toll on individuals and the healthcare system.
Primary care is at the forefront of diabetes prevention, early identification and management. Through focusing on optimal, person-centred care, general practices can continue to significantly improve outcomes and quality of life for people living with diabetes.
This QI toolkit empowers your practice to review data, refine procedures and processes and drive better outcomes for patients on the diabetes care continuum.
This QI Toolkit relates to the following PIP QI Quality Improvement Measures (QIMs):
- QIM #1: Proportion of regular clients with diabetes with an HbA1c result recorded in their GP record within the previous 12 months.
- QIM #5, the proportion of regular clients with diabetes with an influenza immunisation status recorded in their GP record within the previous 15 months.
QIM #1: HbA1c recorded (Type 1 diabetes)
As of July 2024, the CCQ region reported 59.4% of regular clients of all ages who had a recorded diagnosis of Type 2 diabetes had an HbA1c result recorded within the previous 12 months in their GP record, higher than the 57.3% across Queensland and 56.9% nationally.
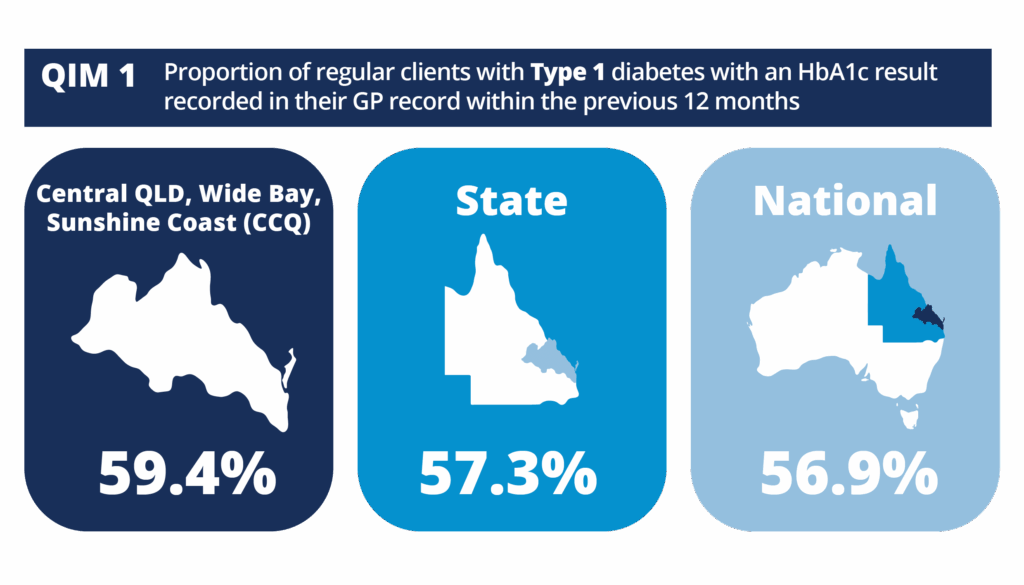
Source: AIHW (accessed April 2025)
QIM #1: HbA1c recorded (Type 2 diabetes)
As of July 2024, the CCQ region reported 72.7% of regular clients of all ages who had a recorded diagnosis of Type 2 diabetes had an HbA1c result recorded within the previous 12 months in their GP record, higher than the 71.5% across Queensland and 71.8% nationally.
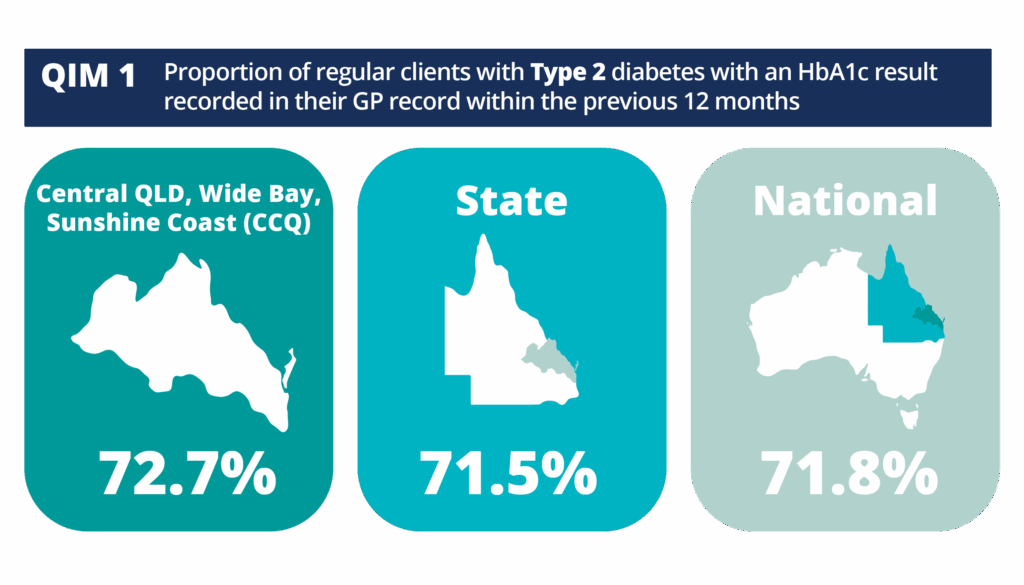
Source: AIHW (accessed April 2025)
QIM #1: HbA1c recorded
(undefined diabetes)
As of July 2024, the CCQ region reported 68.6% of regular clients of all ages who had a recorded diagnosis of Type 2 diabetes had an HbA1c result recorded within the previous 12 months in their GP record, higher than the 64.3% across Queensland and 65.4% nationally.
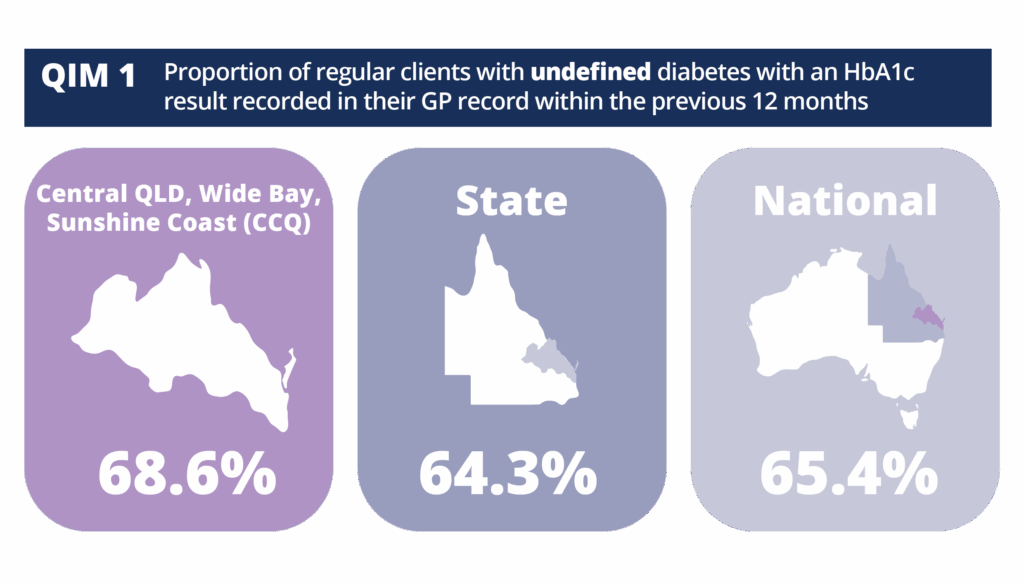
Source: AIHW (accessed April 2025)
QIM #5: Influenza vax recorded (diabetes)
As of July 2024, the CCQ region reported 50.6% of regular clients with diabetes had an influenza immunisation status recorded in their GP record within the previous 15 months in the CCQ region, higher than the 49.7% across Queensland and 48.4% nationally.
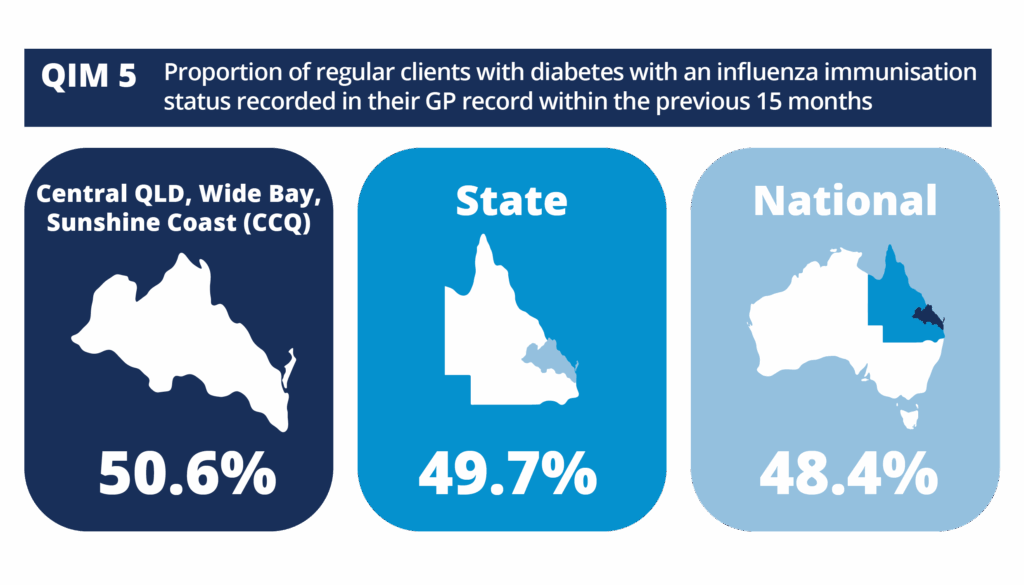
Source: AIHW (accessed April 2025)