Despite osteoporosis affecting over one million Australians and costing the health care system over $3 billion, it remains a largely undiagnosed and under-treated disease.1 In 2023, more than 193,000 fractures occurred in Australia due to poor bone health, many of which were preventable.2
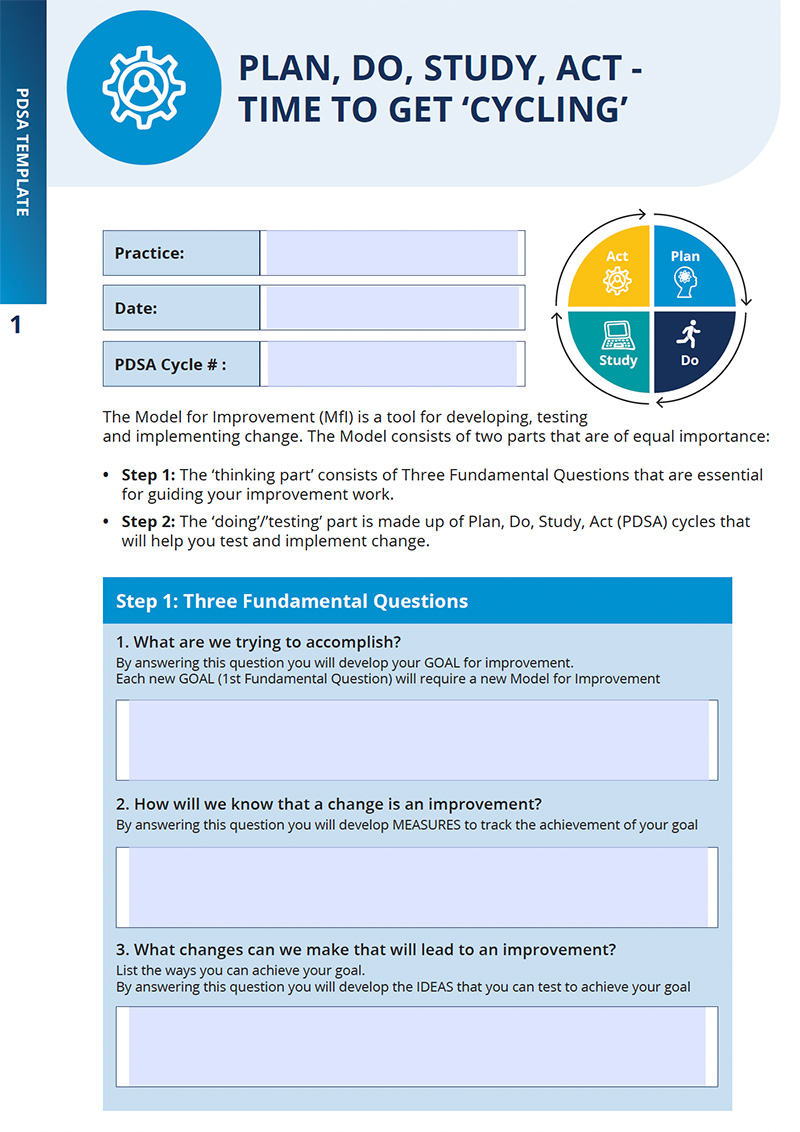
Primary care providers play a critical role in the prevention, screening, early diagnosis and optimal management of osteoporosis. This activity focuses on how to increase the screening and early diagnosis of osteoporosis in general practice to optimise management and reduce fracture risk and improve patient outcomes.